The structure of the airway wall is altered in respiratory diseases such as COPD and asthma through a process called remodelling. Remodelling is likely to contribute to airway obstruction (making it harder to breath) and is particularly problematic as, while current COPD and asthma therapeutics can control symptoms, they are not able to fully reverse the remodelling process.
We have identified three major targets as being of interest for the treatment of airway remodelling in asthma fibrosis and lymphangioleiomyomatosis (LAM) – one involves targeting angiogenesis, or new blood vessel formation, another tackles the accumulation of fibrotic proteins in the airway wall in airway disease and the third focuses on the lymphangiogenesis which is abnormal in LAM and could have implications for cancer.
Chronic obstructive pulmonary disease (COPD)
COPD is the name given to range of chronic lung diseases including emphysema and chronic bronchitis. It is often the result of prolonged exposure to irritants such as cigarette smoke or inhaled particulates.
Although COPD was first characterised in the 1800s many questions still remain about why certain stimuli cause COPD, why some people develop COPD over others, and why COPD gets progressively worse even when exposure to noxious stimuli is eliminated. For these reasons current therapies for COPD are limited in both number and efficacy, being unable to reverse or inhibit pathological changes.
We have have developed a novel in vitro model of COPD in which we expose airway cells to cigarette smoke extract (CSE) and examine effects on cytokine and extracellular matrix protein release to help understand mechanisms underlying smoking induced lung tissue destruction and remodelling. John Whitelock at UNSW is bringing his expertise with the protein perlecan to Brian Oliver’s studies in smoking related lung disease and Ian Adcock at Imperial College, UK is an expert in epigenetics.
Understanding cellular signalling in respiratory diseases
Both asthma and COPD are chronic diseases which are characterised by chronicinflammation and airway remodelling. At a cellular level we investigate if the mechanism by which cells respond to external stimuli, the signalling pathways, are overactive and/or are missing the stop signals. For example we are examining the role of one such stop signal, MKP-1, which we know is reduced in severe asthma thus allowing inflammation to continue unchecked. Our research aims to find ways to enhance the levels and/or activity of MKP-1 to provide a novel anti-inflammatory strategy in asthma and airway remodelling.
Respiratory viruses
Twenty percent of the Australian population either have asthma and/or chronic obstructive pulmonary disease (COPD). These diseases are characterised by periods of stability punctuated by acute increases in symptoms, known as exacerbations. Exacerbations occur even when treatment regimens are optimal, and result in substantial morbidity, mortality and health care costs. Human rhinovirus, the common cold virus, is a major precipitant of exacerbations of both diseases. In our research we look at both the incidence of virus infections and their association with symptoms in people with asthma to in vitro studies. In our in vitro studies we use innovative models to understand how virus infection affects inflammation and how therapeutics work. We have previously explored the mechanisms underlying decreased functionality of bronchodilators which occurs during viral infections in people with asthma.
Lymphangioleiomyomatosis (LAM)
We have increased our research effort into this deadly disease of young women. We are studying how matrix metalloproteinases (MMPs) interact with the abnormal cells in LAM.
Markus Weckmann (who has returned to the University of Lübeck, Germany following a Post Doc position in the RRG) has extended Sarah Boustany’s observation of a missing fragment of collagen from the lung tissue of LAM patients and has cloned and characterised its properties to find that it inhibits lymphangiogenesis and proliferation of LAM cells. We will continue to examine biological samples obtained from LAM patients participating in a trial of doxycycline at St Vincent’s Hospital, Sydney for content of MMPs and their inhibitors – tissue inhibitors of MMPs or TIMPs. Mike Berridge and James Baty from the Malaghan Institute of Medical Research, Wellington, New Zealand are examining the self-renewing properties of LAM cells.
Maria Sukkar Pattern-recognition receptors and the pathogenesis of chronic airways disease: Damage to the airway tissue by common environmental exposures such as inhaled allergens (eg. house dust mite) and air pollutants (eg. ozone, tobacco smoke) and respiratory infections are strongly implicated in the inception and progression of asthma and/or COPD in genetically susceptible individuals. Repeated tissue injury, chronic inflammation and abnormal tissue repair lead to structural alterations or remodelling of the airway wall, contributing to airflow limitation and variable airflow obstruction. Dr Sukkar leads a research program focused on understanding how the airway tissue ‘senses’ and ‘responds’ to environmental insult; with the aim of targeting these receptors for therapeutic benefit. Her current work is focused on elucidating the role of RAGE (the receptor for advanced glycation end products), a unique pattern recognition receptor involved in the host response to tissue injury, infection and inflammation in chronic airways disease. RAGE recognises and binds to a large repertoire of soluble and cell-associated molecules released/expressed by stressed, injured, inflamed or infected cells and tissues (collectively termed damage-associated molecular patterns or DAMPs) leading to sustained cellular dysfunction. Dr Sukkar is examining the impact of RAGE activation on cellular responses in airway structural cells (epithelial cells, airway smooth muscle cells) in vitro. Through collaborations with Dr Simon Phipps (School of Biomedical Sciences, The University of Queensland) and A/Prof Peter Wark (Centre for Asthma and Respiratory Disease, Hunter Medical Research Institute, The University of Newcastle) she is extending these studies to understand the impact of RAGE activation in animal models of asthma and in patients with chronic airways disease. Current PhD students working on these projects include Md Ashik Ullah, Zaridatul Aini Ibrahim and Sharon Wong.
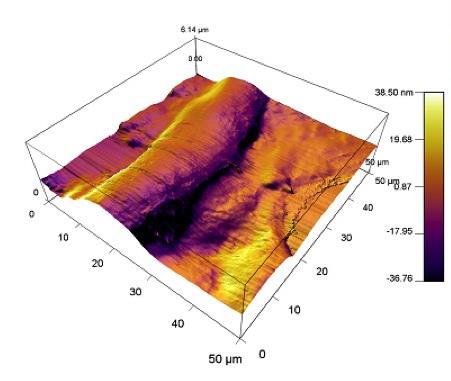
Contraction of human airway smooth muscle grown in collagen gels in response to histamine.
Airway mechanics is investigated by the smooth muscle mechanics group who are interested in the mechanisms of increased airway sensitivity and increased ability to narrow. The group's philosophy is that structure is strongly linked with function and with changes in airway pathology/structure it is not surprising that airways from asthmatic and emphysema patients behave abnormally. Since sensitivity relates to clinical symptoms they believe it is important to understand the mechanism of increased sensitivity.
Pulmonary fibrosis/Interstitial Lung Disease (ILD): Tamera Corte runs the interstitial lung disease clinic at Royal Prince Alfred Hospital and is helping us identify markers of fibrosis in her patients. Hal Collard (San Francisco) provides us with valuable clinical material for our studies on lung fibrosis.